Based on your requests, we’re excited to bring you a transcript of Dr. Seheult’s video on Heart Blocks and Escape Rhythms.
This lecture, which focuses primarily on third-degree AV blocks, offers a sneak peek into our course, ECG Interpretation Explained Clearly. Transcripts like this are perfect to use as a quick reference guide… or if you forget your headphones. Enjoy!
Adapted transcript from Video 22: Blocks and Escape Rhythms, from ECG Interpretation Explained Clearly:
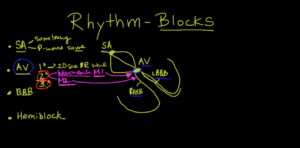
Third-degree / complete heart block basics
We’re gonna discuss third-degree AV block.
This is a complete heart block, where there is basically no communication between the atria and the ventricle.
So, the SA node is still beating, but nothing gets through into the ventricle.
You have the atria beating at one rate and you have the ventricles beating at another rate, and at some point during that time both contract simultaneously.
Because the ventricle is stronger than the atria, it’s gonna close the tricuspid and mitral valves, and you’ll see what’s called the cannon A wave on the jugular venous pulse.
The atria are contracting against a closed tricuspid valve and mitral valve, and that will shoot a column of blood into the jugular venous pulse.
That’s an interesting way of diagnosing or picking this up.
What is a third-degree AV block?
If we look at the AV node, there are basically two ways of having a third-degree AV block, and they can look a little different.
Here we’ve got the AV node, and the AV node goes into the right bundle branch, which goes down this way.
Then, there’s a left bundle branch, but there are two of those.
And so, what you can have is a blockage in either the anterior portion of the AV node, which we’ll call “A,” or the posterior portion, which we’ll call, here, “B.”
This is important, because right in this area is something called the junction which we’ll call “J,” okay?
In other words, there are two different types of third-degree AV block.
You can have a high complete block, or you can have a low complete block.
If the high complete block is up here, then the junction is gonna take over.
If, on the other hand, you have a low block, something in this area, which would be “B.” The junction is gonna be on the wrong side of that block, and instead of a junctional escape rhythm, you’re gonna have a ventricular escape rhythm.
So how does that look?
Let’s talk about “A,” which would be a high third-degree block, or “B,” which would be a low third-degree block.
Well, if you have a high third-degree block, like you would have in “A,” then what you’re you’re going to have an idiojunctional rhythm.
The best way to figure that out is that your QRS is gonna be narrow, because it’s coming from pretty high up.
So you’re still gonna be using the pathway that would make your normal QRS.
So your QRS is gonna look normal.
On the other hand, if you have a low third-degree block, where you’re having the AV node on the “north” side of this block, you’re gonna be using the ventricular escape.
And so, in that situation you’re going to have a wide QRS, okay?
Now, the other way you can tell the difference between this is that, typically, the idiojunctional rhythms are going to have a rate of about 40 to 60 beats per minute.
60, remember, is the lower limit of normal, so this is just gonna be a little bit slower.
Of course, we know it’s a little bit slower; that’s why its overdrive is paced by the atria.
However, the ventricular is gonna be slower, about 20 to 40 beats per minute.
So, how will you know if you have a third-degree AV block?
The atria and the ventricles will be pacing independently of each other.
So, you’ll have P waves going regularly, just like a regular pacemaker would, and this would be at a rate that is commensurate with an atrial rhythm, so 60 to 100.
And then, the ventricles will have their own rhythm, depending on whether it’s idiojunctional or idioventricular escape rhythm.
Let’s say it’s idiojunctional, so it’s a narrow complex.
You’ll see a narrow complex, and then you’ll see another narrow complex. They’ll be going at a rate of 40 to 60 beats per minute.
So you superimpose this electrical finding on top of this electrical finding, and you’ll quickly see that PR intervals are gonna be all over the place. You’ll be able to take a caliper and mark out that the P waves are all equidistant to each other, the QRS complexes are all equidistant to each other, and they’re superimposed.
That’s how you’ll know if it is a third-degree complete block.
How do you know if it’s a “high or low” block?
You can look at the QRS complexes, and if it’s narrow, it’s probably an idiojunctional, or high up, and the rate’s probably gonna be around 40 to 60.
If they’re wide, so almost looking like a PVC, then you’re gonna have a rate of 20 to 40, then it’s probably a bundle branch, or a complete bundle branch, or a low AV node below the junction type of thing, okay?
So let’s take a look at some examples of this type of third-degree AV blocks.
Before we do, however, just be aware of some of the things that you can see in third-degree AV blocks. Think about cannon A waves and why do you get cannon A waves?
You won’t get them all the time, but at one point along the way, this QRS lines up perfectly with a P wave.
You’re gonna be getting the ventricles and the atria contracting at the same time, causing the tricuspid valve to close because the ventricles are stronger than the atria.
And therefore, you’re gonna get the atria contracting against a closed tricuspid valve, and all of that blood – instead of going down into the right ventricle – is gonna go straight up the internal jugular vein, which is gonna cause a huge cannon A wave.
If you see cannon A waves, you wanna think about third-degree heart block.
The other thing that you will see is this AV dissociation.
Now it can be that the ventricles are going so slowly and the atria are not giving any atrial kick, that you could actually have a syncopal event.
That means passing out.
And typically what you’ll need is a pacemaker.
There’s a special term for the syncope in this type of thing that’s called a “Stokes-Adams Syndrome,” so Stokes and then Adams Syndrome.
Examples of third-degree heart block
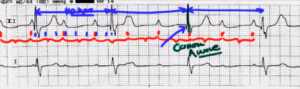
Let’s march out the P waves first, and here’s a P wave, here’s a P wave, here’s a P wave, there.
There’s also a P wave in here if you can’t see it.
Those are the double bump there.
There’s a P wave.
There’s actually, believe it or not, a P wave buried in the QRS complex; that’s why it looks a little bit odd.
And another P wave here and another P wave there.
And you can see very clearly that these P waves are marching, if you will, to the beat of their own drum, which is exactly what they’re supposed to do.
The problem is is that it’s not being conducted through the AV node.
And so, the QRS is seeing something completely different.
What they’re seeing is this rate.
And because of that, that is called third-degree heart block or complete AV dissociation.
So the question is, what is the type?
In terms of the type of block this is, let’s count some boxes here.
So we’ve got one, two, three, four, five, six, seven and probably a half or close to 7.4 here, in terms of the number of boxes.
So, 300 divided by seven and a little bit is around 40 or so beats per minute.
That’s kind of right on the edge, but notice that these QRS complexes are relatively narrow, so this is probably gonna be a higher block, potentially with an idiojunctional rhythm, okay?
So, it’s potentially junctional although this 40 is right on the edge of that.
Now, notice here we’ve got a P wave and a QRS complex happening at exactly the same time.
This would result in a cannon A wave, right there.
Another example of complete heart block
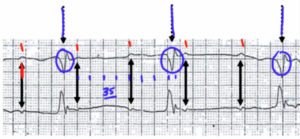
Again, what we have here are P waves, a little bit slower this time.
This case it’s one, two, three, four boxes, and 300 divided by four would be 75.
So looks like the atria are being paced at about 75 beats per minute.
Let’s take a look at the ventricles. Here, we have a ventricle, here, we have a ventricular contraction, and here, we have a ventricular contraction.
So let’s do the math.
We’ve got one, two, three, four, five, six, seven, eight and a half.
Now, that’s around 35 beats per minute, and notice how wide these complexes are. So, this would be more of a lower third-degree AV block in this situation.
Now, just be aware of one possibility.
If you saw a completely flat line without any P waves, that would mean that the SA node had failed and that what we were seeing here is an escape junctional rhythm, which means that the pacemaker is now no longer at the SA node, and it’s no longer at the AV node, but it’s at the bundle branch or ventricular area.
So if that’s the case, we would call that downward displacement of the pacemaker.
This has nothing to do with third-degree heart block; this just has to do with the fact that the SA node is not working and neither is the AV node. So, don’t be confused.
For you to have third-degree AV block or third-degree block or AV dissociation, you’ve got to have evidence of both atrial electrical stimulation and you also have to have evidence of ventricular electrical stimulation.
So let’s review again. We have the AV node first-degree AV block, second-degree AV block, and we just got done with third-degree AV block, specifically the two types.
There is the idiojunctional rhythm, and over here it would be a ventricular rhythm.
So, the junction which is right here at “J,” is what’s causing you to have these narrow complexes.
And then the rate, 40 to 60, which is the higher one would be the idiojunctional rhythm and 20 to 40, which would be the slower would be ventricular.
Thanks for joining us.
