The following is a transcript from Roger Seheult, MD’s video lecture on Chronic Cough Explained Clearly:
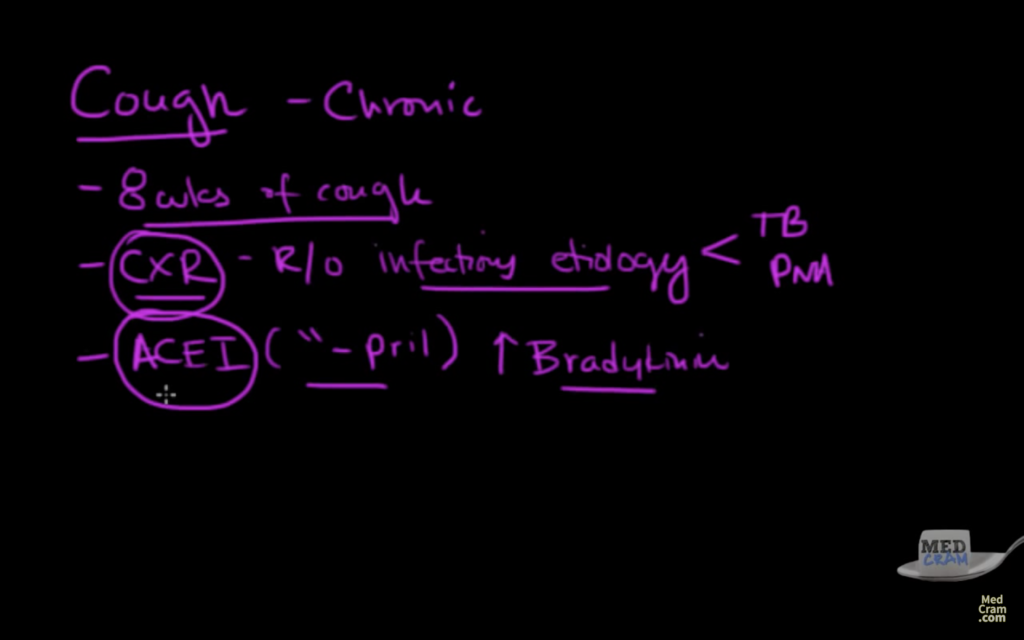
Welcome to another MedCram lecture. We’re going to talk about chronic cough. This is defined as a at least eight weeks of a cough. The first thing you want to do if this is going on is generally speaking, get a chest x-ray and rule out infectious etiology. This is a big problem. If you’ve got an infectious etiology, you’re thinking about things like tuberculosis. You’re thinking about pneumonia. This is stuff that you ought to have the physician do right off the bat to rule that out. Let’s just say you’ve got a normal chest x-ray and the other thing you want to rule out is to make sure you’re not on something called an ace inhibitor. That’s a medication that usually ends in a pril. Like Captopril, Lisinopril, Enalapril, Ramipril. These ace inhibitors can cause cough by increasing bradykinin.
First thing to do if someone has chronic cough
Really, if somebody’s got a chronic cough that you’re trying to work out on a test, the first thing you want to do is make sure you’ve got a chest x-ray to rule out infectious problem and then look at their med list to make sure they’re not on an ace inhibitor. I would say about 30% of patients with an ace inhibitor are going to have some sort of a chronic dry cough. Once you’ve ruled these out, what are the possibilities? Let’s talk about what those possibilities are.
Three possibilities in terms of chronic cough
Three possibilities that I like to look at in terms of chronic cough. The first thing I’d like to do is start off with one from the top if you will. If you know you’ve got, here’s my little picture here of a head, the nose, the mouth. You know that the nasal passageway goes down this way and you’ve got your tongue.
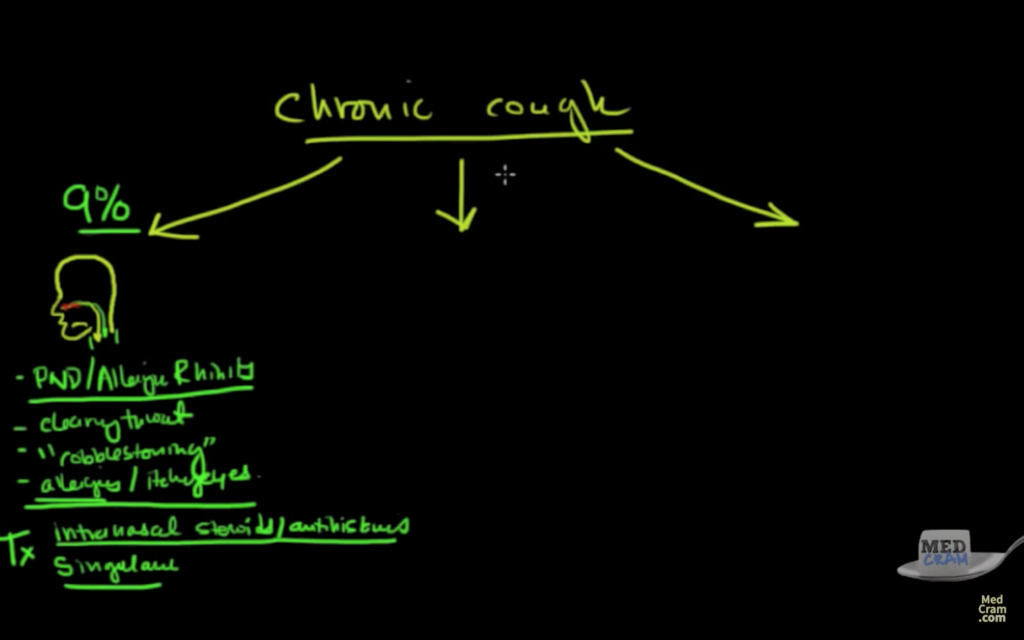
Chronic cough / PND allergic rhinitis
If you’ve got allergic rhinitis in this area, you’re going to make a lot of secretions and those secretions are going to pool and then tickle down into the back of the throat, and it’s going to cause you to clear your throat. That’s what we call post-nasal drip or allergic rhinitis. Post-nasal drip, allergic rhinitis. What are the symptoms of that? Clearing your throat a lot. If you look in the back of the throat, you see this thing called cobble stoning. You’ve got itchy eyes or allergies, itchy eyes. Think about all those things in terms of post-nasal drip or allergic rhinitis. I would say out of all the people who have a chronic cough, or what we’ve eliminated, this accounts for about 9% of that. Think about that the next time someone comes in with a chronic cough. It’s quite possible that we could be dealing with someone with post-nasal drip.
What’s the treatment for that? Well, you want to try to identify the things that’s causing the allergies, but the treatment generally speaking is intra-nasal steroids. Okay, so you’ve heard of things like Nasonex. You’ve heard of Flonase. You’ve heard of Astelin or Astepro. These all kind of intra-nasal steroids or antihistamines. The other thing that’s indicated for allergic rhinitis is Singulair. That might be something else that you could use for a possible chronic cough. If those symptoms fit, that’s great.
Okay, let’s go onto the next possibility.
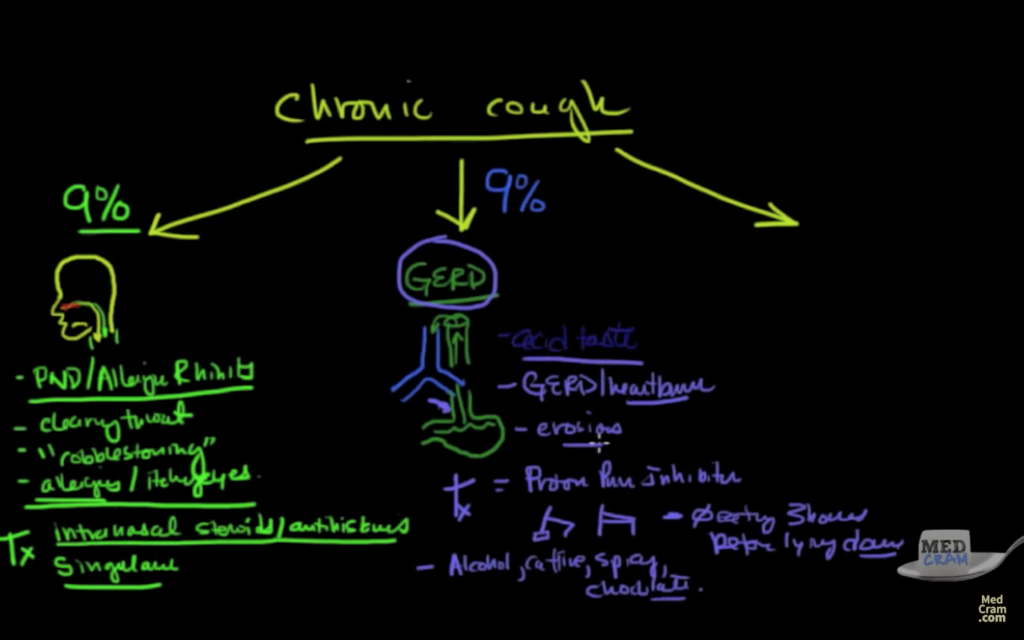
Chronic cough / GERD
The next possibility is also around 9%, instead of coming from the top down, it comes from the bottom up. Here you’ve got your airway, but right next to your airway, in fact right behind your airway is your esophagus which goes down to your stomach. If you’ve got stuff in there and you get something called gastroesophageal reflux disease. It can sometimes come in and irritate that airway and cause what we call GERD.
Where do we see GERD occurring? GERD is occurring or GERD related cough can happen actually in young people. You don’t have to be old. Typically what you see is an acid taste in the morning, let’s lighten that up here so you can see it a bit better. An acid taste in the morning. You obviously have the symptoms of gastroesophageal reflux disease, that’s heartburn. Sometimes you might have erosions from the acid in the back of your throat, or specifically in your teeth, you might have erythema there. If someone were to look down into your throat, like an ear, nose and throat physician, they’d see that it’d be erythematous. What is the treatment for that? You can use a proton pump inhibitor. You can actually get that over the counter called Prilosec or you can get Protonix, pantoprazole. There’s so many different types of proton pump inhibitors.
There’s some other things that you can do. You can take the head of your bed and put it on two bricks, so that it’s facing up. Alternatively, you could also get a wedge. The purpose of this is to keep the head of your bed up, so that the abdominal contents don’t come up and bathe the trachea. They stay down. Other things that you can do is no eating three hours before lying down. Then there’s the sphincter which is right here at the stomach and there are a few things that we know about that can cause that sphincter to open up and you want to avoid those things. Those things that we would avoid, especially at night would be alcohol, caffeine, spicy foods and chocolate. If that seems to be, what seems to be fitting in there GERD, then these are the kinds of things that you might want to make sure that you’re not doing.
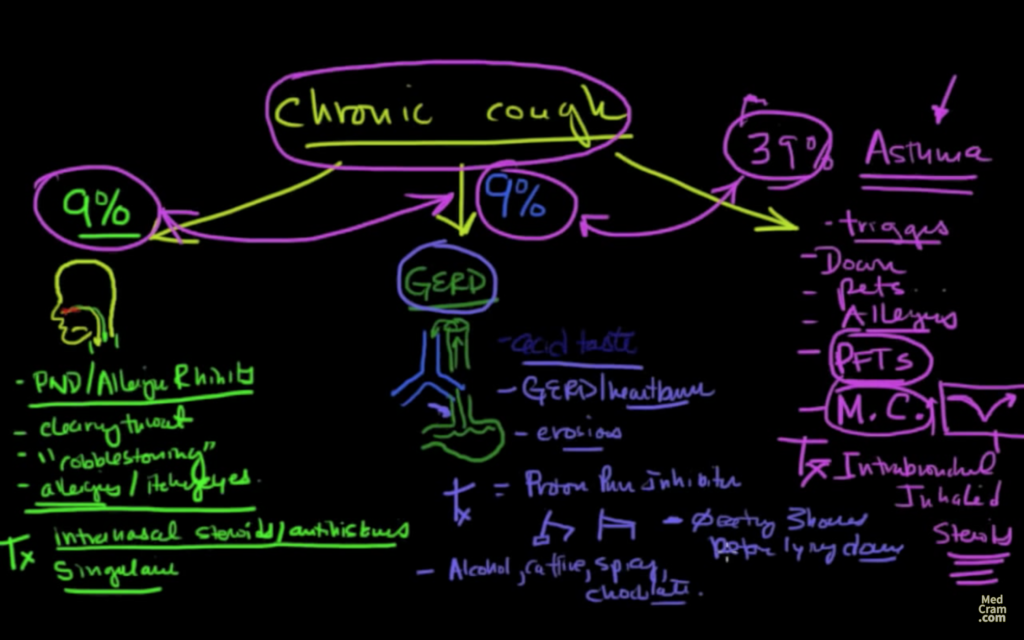
Chronic cough / Asthma
The last one is probably the most common. This is about 39%. This is probably the majority and that’s asthma. Okay, so they don’t wheeze, they just cough, or maybe they do wheeze, but they don’t have to. Just coughing could be a symptom of asthma. That alone might do it. What are these types of patients? They’re going to have the symptoms of asthma, except instead of wheezing, they’ve got a cough, so there’s going to be triggers. Maybe they’ve got down feather pillows or down feather comforters, so look for triggers like down, or pets in the bedroom, or allergies. You’re not going to really know that this is what’s going on, unless you do a pulmonary function test. Now look at the Med Cram lectures on pulmonary function tests to get some idea of what asthma should look like.
Then the other thing, the most diagnostic thing that you will do is a methacholine challenge test. This is where they take in a breath and do an FEV1 maneuver and then you give them methacholine and you see how they do. If they drop down, then you know that they are susceptible to methacholine, which means they’re asthmatic. Then you give them an Albuterol treatment and they come back up again. If that happens then you know the methacholine challenge test was positive, then it’s asthma you’re talking about. If that’s the case, then you’re going to use intra or inhaled, intra-bronchial or inhaled steroids. That’s exactly how you treat asthma. Here’s the trick though, most of the time this chronic cough is not due to just one of these. It’s actually due to multiple.
You’ll see that there’s overlap between these different areas. You might have to employ different treatments in all of these different places. Think about that the next time you have a patient with chronic cough. Think about cough variant asthma, which is this one. Think about gastroesophageal reflux disease which is this one and think about allergic rhinitis, which is that one. Thanks very much.
If you would like to view the full video of this blog, please click on the link below.
Chronic Cough Explained Clearly
